By: Alyx Hewlett, BA
Since 1951, the Canadian Mental Health Association (CMHA) has hosted Mental Health Week every first week of May. This week, communities, schools and workplaces gather to celebrate and promote mental health. Each year there is a different theme: this year’s theme, and the focus of this blog post, is empathy.
Mental Health and Stigma in Canada: An Overview
Mental health is a worldwide public health issue. According to the Government of Canada, 1 in 3 Canadians will be affected by a mental illness in their lifetime; that is approximately 9.1 million people in Canada alone (2020). While there has been an increase in the availability and accessibility of mental health services in Canada, research suggests that there are still significant barriers that prevent Canadians from accessing and receiving appropriate mental health care services (Ferreira & Ross, 2021). One of the primary barriers is the stigmatization of mental health (Rüsch, Angermeyer & Corrigan, 2020). Stigma can be a barrier in itself – that is, self-stigmatization of mental health may prevent people from seeking treatment. However, fear of stigma is also a barrier to accessing mental health services, as these individuals (called “potential consumers”) try to avoid public stigma by not pursuing treatment or other psychiatric services (Rüsch, Angermeyer & Corrigan, 2020).
There are many ways to combat stigma, such as learning (and using) less stigmatizing language in social interactions, acknowledging one’s perceptions of the stigmatized group (such as individuals with substance use disorders), and promoting open communication (Judd et al., 2021). However, this blog post will focus on the 2022 Mental Health Week theme of empathy in overcoming stigma, mental health and substance use disorders, and practicing self-care.
For more information about stigma and discrimination: ontario.cmha.ca/documents/stigma-and-discrimination/
For more statistics on mental health prevalence in Canada: health-infobase.canada.ca/datalab/mental-illness-blog.html#:~:text=1%20in%203,illness%20during%20their%20lifetime%202
What is Empathy?
It is essential to understand that empathy is not a means to “fix” someone’s problems. Instead, empathy allows for compassion, understanding, and the ability to see the world through someone else’s eyes.
The Berkeley University of California’s Greater Good Magazine describes empathy as “the ability to sense other people’s emotions, coupled with the ability to imagine what someone else might be thinking or feeling. Affective empathy refers to the sensations we feel in response to another individual’s emotions (Goleman, 2008). This can be shown in a couple of different ways, such as “mirroring” a person’s emotions (i.e., crying because they are crying) or simply feeling stressed or overwhelmed in response to someone else’s anxiety or fear (Goleman, 2008). On the other hand, cognitive empathy refers to an individual’s ability to identify and understand someone else’s emotions (Goleman, 2008).
Empathy can be learned and practiced. According to Harvard’s Dr. Ronald Siegal, “empathy can be cultivated at any time in our lives,” and the purpose of it is to assist us in understanding other people (Siegal, as cited in Corliss, 2021). It allows us to feel more connected and able to help others, especially during difficult times (Corliss, 2021).
According to Harvard Health Publishing’s blog, there are three measures that you can practice on your own to cultivate greater empathy:
- Acknowledge your biases. Even if we are not aware of them, we all have biases or prejudices that can be challenging to recognize. This includes conscious biases (that is, biases that we are aware of) and unconscious biases that are more challenging to determine. Common unconscious biases are perpetuated by differences in gender, race, weight, class, age, and culture. While unconscious biases are, by definition, beneath our conscious understanding, there are ways to explore them so that they hold less power over us. One such method is through tests, such as this Implicit Association Test (IAT) from Harvard’s Project Implicit: Take a Test (Corliss, 2021)
- Ask questions sensitively. When talking to someone, it is easy to misunderstand them, even if it is someone whose background and identity are very similar to yours. Don’t assume that you know how someone else feels. Instead, ask questions such as “How do you see it?” and “What is your experience?” Acknowledge that your reactions may be different, and express willingness to hear their perspective. This will help them feel respected, and it will help you understand their true feelings. (Corliss, 2021).
- Listen actively. Empathy doesn’t stop after you have asked a question. It is also essential to listen and understand what they say in response. The following three techniques can help you listen more actively:
- Make eye contact. This can help your concentration and improve your connection with the other person. (Corliss, 2021)
- Don’t interrupt. Ensure that the other person is finished speaking before you choose to respond. (Corliss, 2021)
- Avoid suggesting possible fixes unless asked for. If the individual you are speaking to is demonstrating negative emotions about a situation, only offer potential solutions if the advice is requested. (Corliss, 2021)
For more information on the steps above and other means to cultivate and practice empathy, visit Harvard’s blog post here or Berkeley University of California’s informational blog on practicing and developing empathy here: Empathy Definition | What Is Empathy. For more information on active listening, visit CMHA’s checklist here: mentalhealthweek.ca/how-to-really-listen-a-checklist/.
Empathy and Stigma
Empathy and stigma are, in a way, opposites. Where empathy is the capacity of an individual to understand the emotions and feelings of another, stigma is defined as “a sign of disgrace or discredit, which sets a person apart from others” (Byrne 2000, as cited in Ring & Lawn, 2019). Empathy training alone is not likely to change attitudes toward certain groups, such as individuals with borderline personality disorder (BPD) (Ring & Lawn, 2019). However, in cases such as patients with BPD, mental health professionals may have less empathy towards their clients due to negative preconceptions of BPD, such as viewing people with BPD as manipulative, or as individuals with “bad behaviour” rather than behaviour caused by an illness (Ring & Lawn, 2019). Additionally, there is poor health literacy regarding patients with BPD (Lohman et al., 2017, as cited in Ring & Lawn, 2019). This barrier leads to misconceptions by mental health professionals, such as patients being seen as manipulative or attention-seeking rather than “truly” mentally ill (Sulzer, 2015, as cited in Ring & Lawn, 2019). While this example deals primarily with the stigmatization caused by misconceptions about BPD, it is important to be aware of potential misconceptions and literary barriers regarding other illnesses, as well.
Because of these negative issues, researchers have argued that mental health professionals are more likely to be less empathetic or withhold empathy when working with patients with disorders such as BPD (Fraser & Gallop, 1993, as cited in Ring & Lawn, 2019). Empathy is therefore encouraged as a process of overcoming frustration, anxiety, and stigmatization that may arise from working with patients with BPD or other disorders (Chugani, 2016, as cited in Ring & Lawn, 2019). Suggestions to increase empathy include providing consistent professional supervision and stressing the importance of self-reflection in increasing self-awareness of negative reactions to patients (Millar et al., 2012, as cited in Ring & Lawn, 2019).
Empathy in Addiction and Substance Use Disorders
While empathy is indeed important in understanding and helping people with various mental health disorders, it may also play a role in the influence of substance use trajectories and recovery (Massey, Newmark & Wakschlag, 2017). Researchers Massey, Newmark and Wakschlag have illustrated a hypothesized schematic of how varying degrees of empathic capacity might influence the progression of substance use either positively or negatively (Massey, Newmark & Wakschlag, 2017). This simplified illustration is included below. It outlines the hypothesis that empathy impairments (particularly affective empathy impairments) could reduce sensitivity to environmental triggers that discourage the escalation of substance use (Massey, Newmark & Wakschlag, 2017). As a result, affective empathy impairment could potentially enable a progression towards addiction, and high empathy could potentially prevent initial use or reduce the likelihood of use progressing into problematic use or addiction.
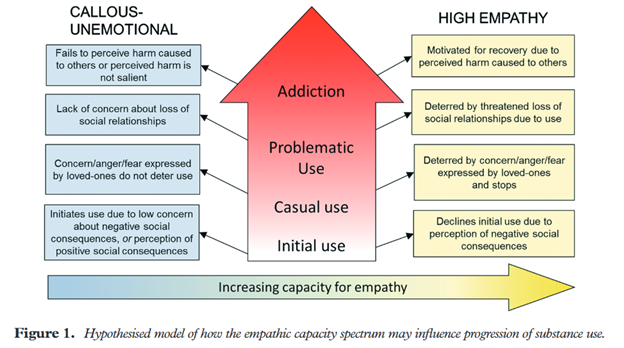
Figure 1 taken from Explicating the role of empathic processes in substance use disorders: A conceptual framework and research agenda. Massey, Newmark & Wakschlag, 2017.
Empathy in Therapists and Practicing Self-Care
Empathy is not only important in preventing and treating mental health and substance use disorders. In a 2013 Swedish study, researchers examined the “butterfly effect of caring,” which is essentially the practice of compassion towards oneself as a building block to compassionate care for others (Raab, 2014). Research suggests that therapists with low self-compassion and high self-criticism are more critical of their patients, resulting in poorer patient outcomes (Raab, 2014). Low empathy and compassion impact the client-clinician relationship, which consequently affects the therapist’s well-being (Raab, 2014). According to Todaro-Franceschi (2013), nurses who are “seemingly heartless” and exhausted will be dispassionate in caring and therefore will not feel good about themselves, leading to constant exhaustion and belief that their job is not being done well. Additionally, they will often feel disheartened, hopeless, joyless, and numb (Todaro-Franceschi, 2013, as cited in Raab, 2014).
Research has discovered that mindfulness interventions hold beneficial potential in reducing burnout and stress and increasing empathy and self-compassion (Raab, 2014).
Observing Mental Health Week
There are various ways you can recognize and promote Mental Health Week. To learn more, view the Mental Health Week 2022 Toolkit provided here: https://www.mentalhealthweek.ca/2022-toolkit/
Resources Compiled:
https://www.mentalhealthweek.ca/
https://mentalhealthactionplan.ca/tools/mental-health-training-framework/mental-health-awareness/
https://mentalhealthcommission.ca/resources/
https://www.mentalhealthweek.ca/how-to-really-listen-a-checklist/.
References
Corliss, J. (2021, February 22). Want to feel more connected? Practice empathy. Harvard Health Publishing. Retrieved April 29, 2022, from https://www.health.harvard.edu/blog/want-to-feel-more-connected-practice-empathy-2021022221992#:~:text=%E2%80%9CEmpathy%20requires%20paying%20attention%20to,Siegel
Ferreira, V. B., & Ross, E. (2021). An Intersectional Approach to Understanding the Barriers of Accessing Mental Health Services in Canada. Western Undergraduate Psychology Journal , 9(1), 35–43.
Goleman, D. (2008, March 1). Hot to Help. Greater Good Magazine. Retrieved April 29, 2022, from https://greatergood.berkeley.edu/article/item/hot_to_help
The Greater Good Science Center. (2022). Empathy definition: What is empathy. Greater Good Magazine. Retrieved April 29, 2022, from https://greatergood.berkeley.edu/topic/empathy/definition
Judd, H., Meier, C. L., Yaugher, A. C., Campbell, E., & Atismé-Bevins, K. (2021). Correction to: Opioid use disorder stigma reduction through story telling narrative and sharing: A qualitative review and lessons learned. International Journal of Mental Health and Addiction. https://doi.org/10.1007/s11469-021-00639-3
Massey, S. H., Newmark, R. L., & Wakschlag, L. S. (2017). Explicating the role of empathic processes in substance use disorders: A conceptual framework and research agenda. Drug and Alcohol Review, 37(3), 316–332. https://doi.org/10.1111/dar.12548
Public Health Agency of Canada. (2020, October 8). Data Blog: Mental Illness in Canada. Public Health Infobase | Public Health Agency of Canada. Retrieved April 29, 2022, from https://health-infobase.canada.ca/datalab/mental-illness-blog.html#:~:text=1%20in%203,illness%20during%20their%20lifetime%202
Raab, K. (2014). Mindfulness, self-compassion, and empathy among health care professionals: A review of the literature. Journal of Health Care Chaplaincy, 20(3), 95–108. https://doi.org/10.1080/08854726.2014.913876
Ring, D., & Lawn, S. (2019). Stigma perpetuation at the interface of Mental Health Care: A Review to compare patient and clinician perspectives of stigma and borderline personality disorder. Journal of Mental Health, 1–21. https://doi.org/10.1080/09638237.2019.1581337
Rüsch, N., Angermeyer, M. C., & Corrigan, P. W. (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry, 20(8), 529–539. https://doi.org/10.1016/j.eurpsy.2005.04.004
